Introduction
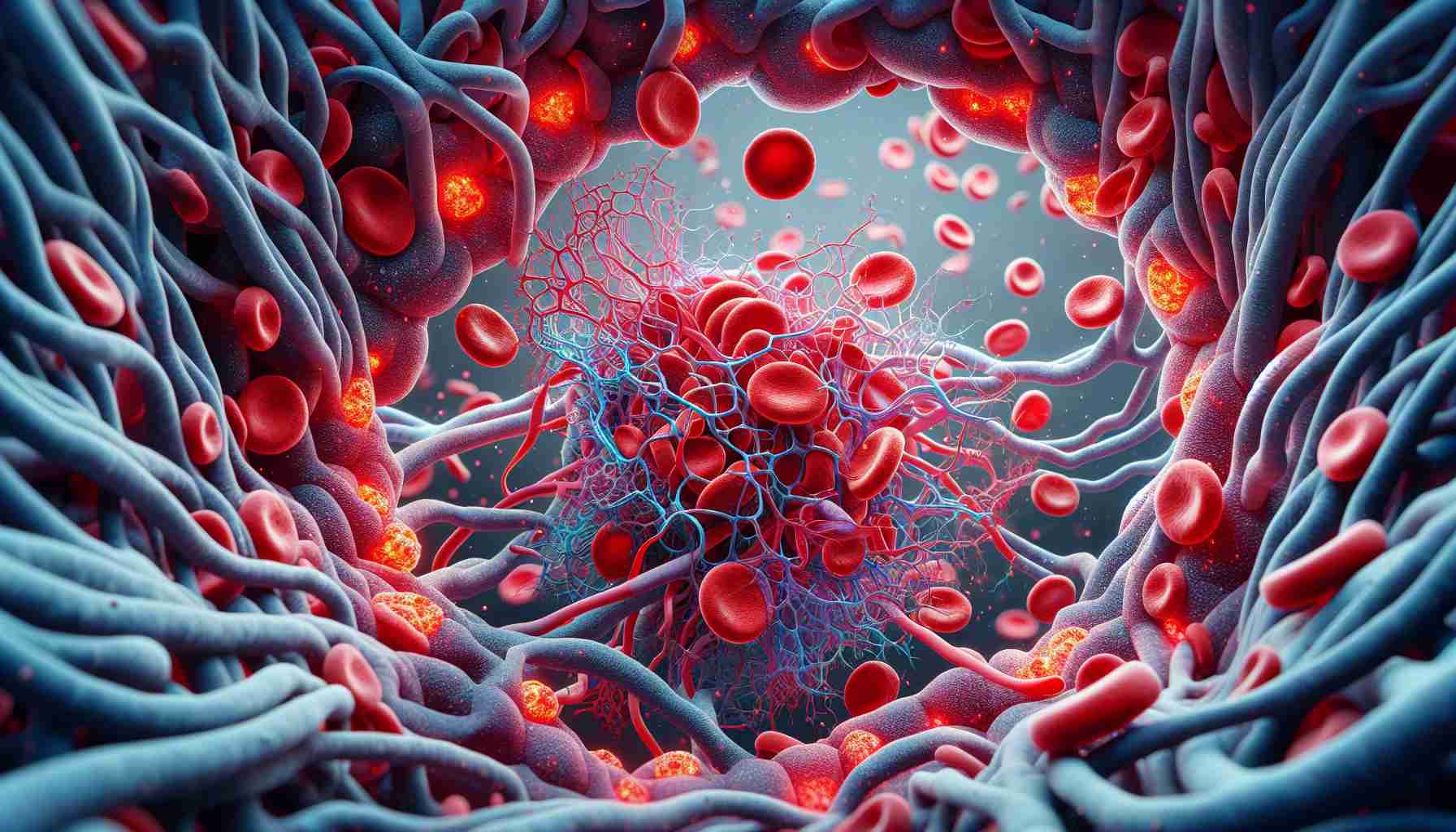
Hemostasis, or blood clotting, involves a balance between coagulation (formation of a clot) and fibrinolysis (breakdown of the clot), which prevents bleeding and maintains healthy blood flow through the arteries supplying essential nutrients to organs. Disease or injury can cause an increase or deficiency in clotting factors such as fibrinogen or thrombin, which can lead to serious complications. Fibrinogen, the main structural component of the blood clot, polymerizes into a fibrin network that surrounds the cellular components of blood and aids in wound healing. Clotting begins when blood vessel damage activates platelets and transforms proenzyme thrombin (Factor II in the coagulation cascade) into active thrombin. Thrombin cleaves fibrinopeptides from fibrinogen, creating fibrin monomers with available sites for polymerization. This cycle continues through lateral aggregation and packing, forming fibrin fibers and eventually forming a polymerized fibrin network. Key structural differences between clots formed under different conditions include the density of the fibrin network, pore size, fiber diameter, and fiber number in a given region. Changes in fiber diameter result from lateral aggregation of fibers. If clot formation occurs slowly, as is the case with lower thrombin concentrations, fibers have more time for lateral aggregation, resulting in thicker, longer fibers. Conversely, increased fibrinogen concentration leads to thicker fibers and denser networks. Pores, or openings, in the fibrin network form when individual fibers intertwine, creating a network through which lytic agents can diffuse or penetrate during clot breakdown. These pores occur not only in fibrin clots but also in clinical thrombi and clots made from whole blood. Structural changes in the fibrin network alter the susceptibility or resistance of the clot to breakdown.
Fibrinolysis is initiated when plasminogen activator, most commonly tissue plasminogen activator (tPA), converts plasminogen into plasmin. Plasmin then binds to fibrin and crosslinks the fiber by enzymatic degradation. Elevated tPA levels are believed to be a result of injury, coagulation cascade activation, endothelial activation, exercise, and disease. Additionally, altered tPA concentration is considered a risk indicator for myocardial infarction. Internal fibrinolysis occurs when tPA molecules are trapped within the clot during its formation and initiate fibrin degradation within the clot. Currently, it is unknown what structural changes occur during clot breakdown.
When a clot cannot be dissolved solely by internal fibrinolysis, such as in the case of a heart attack or stroke, tPA is delivered exogenously in a process called external clot lysis. Modeling simulations of external fibrinolysis, supplemented with experiments, have shown that the ratio of tPA molecules to fibrin is crucial for efficient clot breakdown. The composition of the clot can inform tPA dosage for patients to prevent excessive bleeding and effectively treat the patient within an appropriate time window. However, this discovery has only been reported for external fibrinolysis and has not yet been explored for internal fibrinolysis. A better understanding of the role of protein concentrations and clot structure in internal fibrinolysis behavior may aid in refining external fibrinolysis and advancing clinical progress.
The diameter of fibrin fibers, network density, and other clot structure parameters can facilitate or hinder clot dissolution.
Frequently Asked Questions (FAQ) based on the main topics and information presented in the article:
Question: What is hemostasis?
Answer: Hemostasis is the process of blood clotting and clot dissolution, which prevents bleeding and maintains healthy blood flow through arteries supplying nutrients to organs.
Question: What are the causes of normal clot formation?
Answer: Clot formation involves blood vessel damage, platelet activation, and the transformation of proenzyme thrombin into active thrombin. Thrombin forms fibrin fibers that surround the cellular components of blood, creating a clot.
Question: What are the key differences between clots formed under different conditions?
Answer: Key differences include the density of the fibrin network, pore size, fiber diameter, and fiber number. For example, lower thrombin concentration leads to slower clot formation with wider and longer fibers.
Question: What mechanisms are responsible for clot breakdown?
Answer: Clot breakdown occurs through fibrinolysis, which is initiated by plasminogen activator. Activated plasmin cleaves fibrin fibers through enzymatic degradation.
Question: What factors influence clot dissolution?
Answer: The concentration of tissue plasminogen activator (tPA) can be increased due to injury, coagulation cascade activation, endothelial activation, exercise, and disease. Internal clot dissolution occurs when tPA molecules are trapped within the clot, while external clot dissolution is initiated by the delivery of exogenous tPA.
Question: What are the potential applications of this information in patient treatment?
Answer: Understanding clot structure and protein concentrations can help determine tPA dosages for patients to effectively treat clots and prevent excessive bleeding.
Definitions of terms:
– Hemostasis: blood clotting, the balance between coagulation and clot dissolution.
– Fibrinolysis: the process of clot breakdown by plasminogen activator.
– Thrombin: an enzyme formed through platelet activation that converts fibrinogen into fibrin.
– Fibrin: the main structural component of a blood clot.
– Fibrinogen: a protein that, when transformed by thrombin, forms fibrin fibers of a clot.
Suggested related links:
– www.clotformation.com
– www.hemostasisexplained.com
– www.fibrinolysisexplained.com
The source of the article is from the blog publicsectortravel.org.uk